|
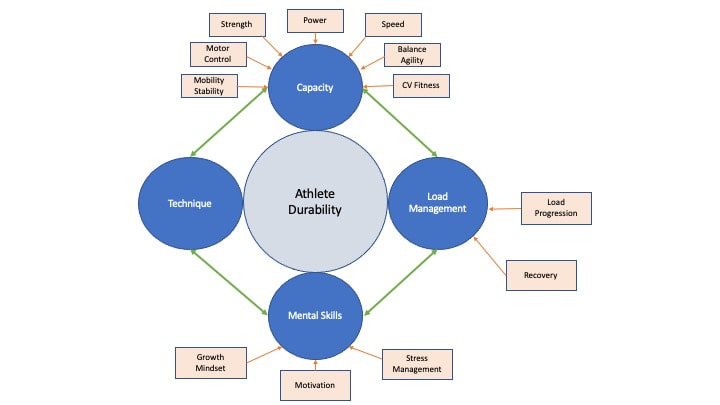
Swimming is considered a relatively safe sport compared to impact sports such as football, but still has its share of injury risks due to its repetitive nature. For example, the prevalence of shoulder injuries among competitive swimmers has been reported to be as high as 91%! How does Physical Therapy help swimmers stay healthy and keep training for peak performance? Minimize Excessive Compensations Our bodies are amazingly adaptable so, if you have limited mobility, strength or motor control in one area, then other parts of your body will learn to move in a new way to get the job done. This is a great system that allows us to keep moving but sometimes the compensations become excessive, and when combined with a rapidly increased training load and/or poor recovery, can lead to overuse injuries. A Movement Assessment by a Physical Therapist helps to identify areas for improvement with your mobility, coordination and strength. This is great information for swimmers of all ages! Young swimmers are constantly growing and growth spurts mean that a swimmer is suddenly using longer arms and legs, and basically has to retrain their neuromuscular control of this “new body”. Older swimmers face similar issues as they might be learning to move with decreased elasticity of tendons, decreased joint mobility, stiff spine or decreased lean muscle mass. Anyone who sits and uses technology for any period of time can start to get tight chest muscles, hamstrings, hip flexors or weak back muscles, glutes or shoulders. Earning the Right to Load So, you want to get STRONG, and you want to swim FAST. Guess what, the best way to do that is lift heavy things and to, you guessed it, swim fast. But, sometimes pain, weakness or immobility cause us to use compensations to do these things. For example, what if the muscles around your shoulder are tight or weak, or your shoulder joint is stiff, and you can’t reach completely overhead? What is going to happen when you try to do an overhead press, waiter’s carry exercise or power snatch? You are going to have to overly arch your back and that means that your trunk is not able to stabilize very well, making it easier to overload your back. What does this look like in the water? When your hand enters the water with freestyle, that arch in your back means that your hips are being pushed toward the bottom of the pool. Taking the time to work on these baseline abilities during your warm up or recovery routine (or during work breaks) help improve your dryland and swimming technique which, in turn, allows you to lift heavier and swim faster. Healthy swimmers keep training and consistent training makes you more durable. Only a small piece of the injury-prevention puzzle Remember that mobility, stability and motor control are merely baseline functional abilities upon which you can build your strength, power, speed, cardiovascular endurance. These are not the only components affecting the durability and resiliency of a swimmer. Looking at the graphic below, you can see there are a number of factors affecting your ability to stay in the game. This may seem daunting but know that everything is interrelated so small changes can have exponential effects. Want to schedule your swim-specific Movement Assessment? Book by 1/31/2023 for a 20% discount
0 Comments
2022 is winding down and now we set our sights on what 2023 will bring. What are your new fitness goals? Have you ever considered a swim vacation? What better way to combine your love of swimming and fitness with your love of seeing the world and trying new things? The number of companies in the swim vacation space has expanded in the last few years with a growing number of locations and experiences Swimming DistanceMost trip itineraries range from 4-5 km per day, but some companies offer "beginner" trips or "short swim" trips. SwimTrek offers trips specifically for beginners with total daily swim distances from 2-3k in locations such as Greece, Mallorca, Hawaii, Turkey and Croatia. BYONS "Bring Your Own Non-Swimmer"SwimQuest and SwimVacation both mention activities for non-swimmers. This can include kayaking, stand up paddle boarding, hiking, riding on the guide boat or even yoga. SwimQuest even provides a tutorial on how to convince your non-swimmer partner that this "swim vacation" will be amazing and offers a 10% discount for non-swimmers. Many of the other companies have limits on how many non-swimmers are included on the trips. AccommodationsAll the swim vacations include accommodations, but that can vary from a cabin on a 30 foot, 20-passenger yacht to a private beachfront residence or hotel. SwimVacation touts some of the more luxurious vacation experiences like this trip to Hawaii that includes a private chef preparing all meals at a beachfront private residence, oceanfront massage therapy, outrigger canoe trip, swimming clinics, other aquatic sport activities and an open bar. LocationsSwimVacation
Tell us about your swim vacation!Have you been fortunate enough to go on one of these swim vacations? Please share your experience and tips in the comments!
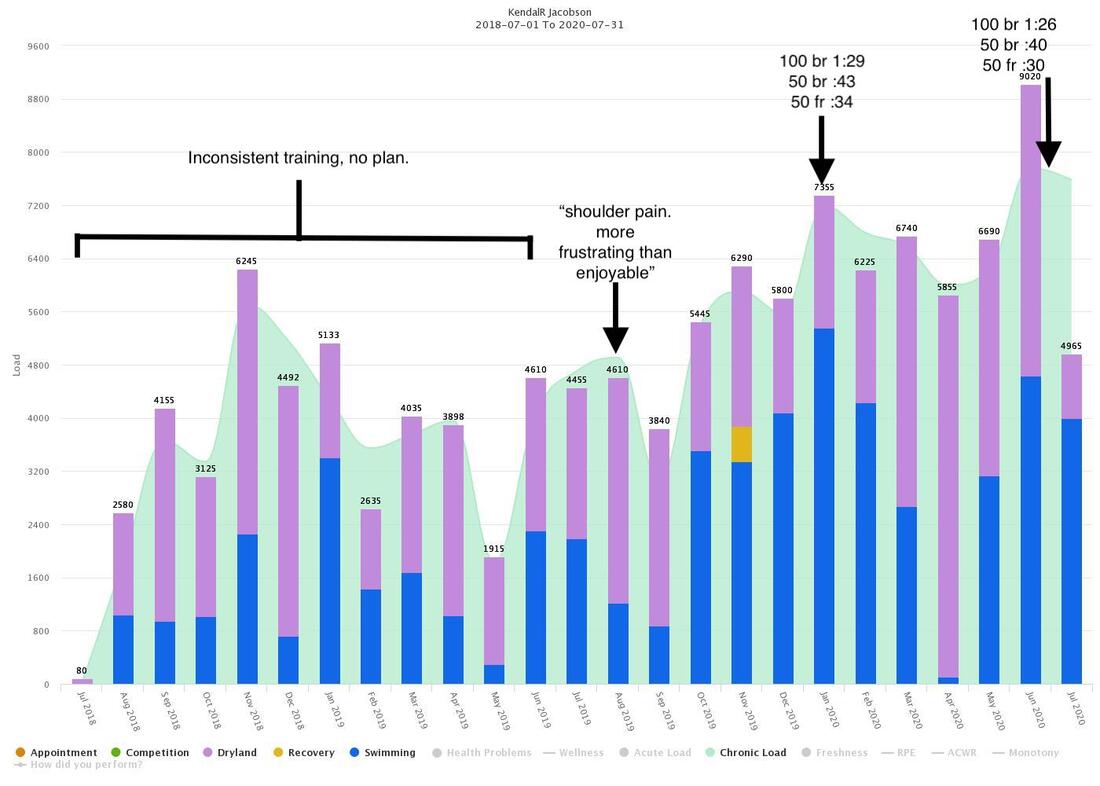
I’ve had a few good swims in the last month. Nothing record-breaking, but definitely worthy of some personal reflection. You know, take a moment to reflect on the journey, celebrate the win and ride the positive momentum. So, I took a stroll down memory lane via my training logs and came across this gem: “Shoulder pain. couldn’t keep up. More frustrating than enjoyable” August 2019 I know I am not alone here. As many as 91% of swimmers suffer from a shoulder injury at some point in their career. How do we end up hurting and frustrated? More importantly, how do we find our way back to swimming fast with less pain? There are many factors that go into making healthy, resilient swimmers. One of the more important factors for masters swimmers, but possibly the MOST DIFFICULT to manage, is training load progression. We are adults and we are busy adulting. Many times our training takes a backseat to pretty much everything. I can guarantee that the majority of things in the front seat are super important: kids, spouses, jobs, oil changes. So, I am not saying that you need to change your priorities, but rather, find opportunities in your daily life to keep you moving toward your fitness goals. Getting stronger and less fragile is accomplished by limiting these huge peaks and valleys in your training load. It makes sense to most people that ramping up your training load too quickly can lead to injuries, but precipitous drops in training can be just as risky. Here is where taking small steps can have the most impact, simply because those small steps keep you moving forward toward your goal. Find ways to throw in some activity every day: a few air squats at work, taking the stairs, walk your meetings, vigorous housecleaning. Committing to doing SOMETHING every day, even if it is only 20 minutes, makes crawling out of the valley a much shorter trip and lets you maximize the time when you do find yourself back in the pool or gym. Do you need help navigating your way back from an exasperating injury? Feel free to contact me kendal@eperformancetherapy.com or 512-736-6742
In this period of social distancing and limited training, NOW is best time to focus on how we can best prepare our athletes to make a safe and productive transition back to their normal training load. This time away is wonderful opportunity to come out of this experience with:
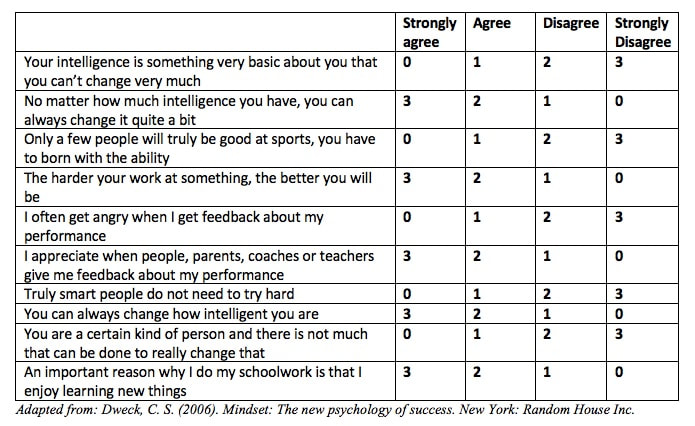
Mindset and Performance As humans we can view challenges in our lives through different lenses that affect our ability to adapt and cope with our situation. How do you look at challenges, adversity or hardship? Take this short quiz. Select the number for each question which best describes you and tally up your score: Score Chart: 22-30= Strong Growth Mindset 17-21= Growth with some Fixed ideas 11-16 = Fixed with some Growth ideas 0-10= Strong fixed mindset Now that you know where you are, now, with your mindset, why does this matter? Well, because developing a growth mindset not only helps you cope with hardship, it makes you WELCOME challenges as an opportunity to learn, grow, improve and excel. This in turn helps you to develop more mental and physical toughness and improve your overall resilience as an athlete. If you don’t believe that you can improve or become better, then you see adverse events as an absolute measure of your worth. For example, I didn't swim as fast as I wanted, so "I am a loser". In contrast, when you face that adverse event with a growth mindset, you look for ways to be prepared for something like it in the future. Instead of beating yourself up, you see at as an opportunity to learn and be better. People with a fixed mindset often fear challenge, avoid effort, and don’t ask for help because their self-worth is wrapped up in their performance. Sabotaging performance is easier than giving a best effort and failing. Asking for help would mean admitting that one is not good enough and lacks the ability to improve. On the other hand, those with a growth mindset can see the value of challenge and effort and welcome help as a means of continually improving. Fixed mindset: Failure = Setback, out of my control Growth mindset: Failure = Opportunity to learn and grow The great news is that our mindset is fluid and can be changed. It is important to be aware of how you are reacting to stress, setbacks, hardships, failures, difficulties, or challenges. Look for opportunities to EXERCISE and develop your growth mindset:
If you go through life only doing things that are easy, was it a life well lived? Training Load as “Protection” From Injury
Training for high performance requires athletes to strategically alternate between increased training load to stimulate physiological responses and decreased training load to allow for adaptation and increased capacity. Interestingly, research on the effect of training load on injury risk shows that high training loads are not only NOT an injury risk, they have been shown to offer PROTECTION FROM INJURY in athletes. Of course, what IS important is HOW you get to those higher training loads. Ramping up intensity too quickly or inadequately recovering between loading cycles pushes an athlete beyond their current capacity and can result in overload at the tissue level (ie tendon injuries) or fatigue-related changes in motor control that can contribute to injuries (not to mention the effects on motivation, concentration, emotional stability, etc). Training at lower loads is also an injury risk because it results in an athlete’s inability to cope with any increases in load. Our goal is to progressively load our bodies to improve our durability; in doing so, we can withstand higher loads for improved performance and decreased risk of injury. Getting the Whole Picture: Training Load and Wellness Sport injuries are dependent on a number of factors. Training load management is not just a matter of calculating extrinsic factors such as training volume, duration and speed, but must also consider intrinsic factors such as heart rate or rate of perceived exertion (“how hard was that workout?”). Internal loads can be affected by a number of things: fatigue, emotional disturbance, poor sleep, poor recovery, illness, or recent training loads. This can explain why the same workout done at one point in the season will feel more or less difficult due to factors such as current fitness level, during a stressful school testing, or after several nights of poor sleep. So, by daily tracking of wellness factors as well as training load factors, we are trying to get a real-time picture of the athlete’s current and past training load, his/her ability to cope with that training load, and his/her readiness to train or compete going forward. Identifying Individual Patterns Research has shown that there is likely an optimal range of load progression to maximize performance and avoid undertraining or overtraining. For example, large week-to-week increases in load have been shown to significantly increase injury risk. Research is showing that an athlete can be at increased risk for injury for 7-28 days following a significant spike in training load! (so, maybe that overuse injury didn’t really come out of nowhere). Another metric used to measure appropriate progressions in load is what is called the acute-to-chronic-workload-ratio (ACWR).
A generalized goal is to keep an athlete’s ACWR between 0.8-1.2. An ACWR of less than 0.8 has been associated with a 5-7% increased risk of injury (undertraining), while an ACWR greater than 2.0 (overreaching) can increase injury risk to 15-20%! This range can vary by sport and individual, so by tracking your own training and wellness data, you can fine tune your training plan according to how YOU specifically respond to changes in training loads. Injury Prevention with Enhanced Performance Therapy Functional Movement Screen Utilizing the Functional Movement Screen and Y-Balance Test (www.functionalmovement.com), we perform functional tests that are used to determine if an athlete is performing at least at a minimal level of “movement competence”. The presence of asymmetries, excessive compensations, painful movements or orthopedic tests, and injury history can indicate an increased risk of a future injury. The results of the screen help to determine what an athlete needs to focus on in their strength training program to improve mobility, stability and motor control with the goal of decreasing compensations that might lead to injury. Training Load and Wellness Tracking Are you interested in bringing this sport science technology to your training? We use a simple data entry web app that you can use from any mobile device or computer. You simply fill out a quick wellness questionnaire every morning, enter daily training sessions, and report the occurrence of any injuries. Results and reporting can be viewed directly from the app and the daily “Ready to Perform” score is visualized using an easy to interpret “stoplight” system. Over time you accumulate more data and will be able to view your Acute:Chronic Workload ratio in real-time for a more sensitive measurement of your workload progressions and the relationship to your wellness scores and onset of injuries. By tracking patterns, you can then make adjustments to your training and/or your recovery strategies based on your own history. We provide educational resources and exercise/self-care interventions via the application based upon your individual needs. Interested in more information? Go to www.eperformancetherapy.com/sports-wellness.html or contact me at kendal@eperformancetherapy.com. References Blanch P, Gabbett TJ. Has the athlete trained enough to return to play safely? The acute:chronic workload ratio permits clinicians to quantify a player's risk of subsequent injury. Br J Sports Med Published Online First: 23 Dec 2015. doi:10.1136/bjsports-2015-095445 Gabbett TJ The training-injury prevention paradox: should athletes be training smarter and harder?Br J Sports Med Published Online First: 12 January 2016. doi: 10.1136/bjsports-2015-095788 Shoulder overuse injuries are very common within the swimmer population whether it be high school, college or masters level participation. A study published in 1995 reveals that 47% of collegiate swimmers and 48% of masters swimmers report experiencing shoulder pain lasting 3 weeks or more.[1] More recently, studies have shown as high as 91% of swimmers aged 13-25 reporting shoulder pain, 84% of those had positive impingement signs, and 69% of those studied with MRI had supraspinatus tendinopathy.[2] One adaptation seen with swimmers experiencing shoulder pain is a decrease in active upward rotation of the scapula with shoulder elevation following a fatiguing bout of swimming.[3] Possible causes for this adaptation can be tonic or shortened levator scapula, weakness of serratus anterior, immobile and kyphotic thoracic spine, weak or fatigued infraspinatus, and adaptively shortened pectoralis minor. Other possible factors contributing to impingement symptoms or overuse tendinosis among swimmers include strength imbalances between subscapularis and infraspinatus, and activation imbalances between upper trap and lower trapezius. In an effort to maintain healthy shoulders in swimmers, it is important to remember that the shoulder girdle articulates with the rib cage and, therefore, the rest of the trunk. So the posture and dynamic control of the trunk can influence how well the shoulder functions. The classic standing “swimmer posture” is characterized as a head forward posture, rounded shoulders, increased lumbar lordosis, genu recurvatim (hyperextended knees), kyphotic thoracic spine (rounded upper back), and flared lower ribs. This posture can lead to poor abdominal and gluteal activation, not to mention altered breathing efficiency and dysfunctional shoulder mechanics. When the shoulders are rolled forward, the shoulder socket is angled downward and the muscles that stabilize the shoulder "ball" in the "socket" (rotator cuff muscles) have to work much harder. The rotator cuff is susceptible to fatigue due to the sheer number of revolutions that occur with a typical swim workout, no need to overload those same muscles with faulty posture. When attempting to strengthen the scapular retractors and depressors, a common compensation for a stiff thoracic spine and poor mid/lower trapezius activation is to further extend the lumbar spine. If a swimmer is only able to retract or depress the scapulae by extending the lumbar spine, this has adverse consequences in the water. When swimming, the hips will drop, the abdominal muscles will be harder to recruit; making the body position less hydrodynamic and the trunk a less stable base for propulsion. Here are some examples of exercises to address some of those typical areas of tightness, immobility or weakness associated with the classic "swimmer posture". This content is for informational purposes only and does not constitute medical advice; the Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of a physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. Thoracic Extension Self-Mobilization Purpose: increase mobility of thoracic spine, decrease kyphotic postures Instructions: Lie on back with knees bent and foam roller behind mid back with foam roller perpendicular to spine. Support neck by clasping hands behind neck with elbows straight forward. Stretch upper back into extension over roll by reaching elbows upward. Pressure on, pressure off. 3-4 reps in 2-3 different positions along mid back. NOTE: Important to keep pelvis tucked under with abs activated in order to avoid excessive lumbar extension. Pectoralis Stretch on Foam Roller Purpose: Stretch pectorals, facilitate posterior pelvic tilt and normalize lumbar extensor tone, increases abdominal activation Instructions: Lie on back on foam roller with knees bent and flat on floor. Inhale with arms in front of face with elbows bent. Exhale, tucking pelvis under and closing ribs as you bring arms into "goal post" position. Inhale to start position. Quadruped Belly Lift with Upper Extremity March Purpose: Facilitate posterior pelvic tilt, activate abdominals with rotational stabilization, close down the ribs to allow diaphragm to relax and normalize psoas tone, and activation of serratus anterior Instructions: Start on hands and knees. Inhale. Exhale and tuck pelvis. Inhale holding tuck. Exhale lift knees and tuck further. Inhale, holding tuck. Exhale, tuck further and lift R hand without twisting or leaning. Inhale and lower hand. Alternate hands. Supine Scapular Overhead Press with Tubing Purpose: Re-educate and strengthen the serratus anterior without thoracic compensations for optimal upward scapular rotation. Instructions: Lie on back with knees bent and feet flat. Tubing wrapped around back with an end in each hand. With arms straight and arms angled slightly upward toward head. Keep pelvis tucked under and press shoulders away from floor and slowly return to start. Prone Scapular Combo on Stability Ball with Posterior Pelvic Tilt Purpose: Facilitate posterior pelvic tilt and abdominal recruitment, facilitate lower trapezius activation without over-activation of upper trapezius, and strengthen infraspinatus. Instructions: Prone over stability ball with body in a plank position Tuck pelvis under and engage abs, "pressing pubic bone into ball". Start with arms at side with palms in. Squeeze blades down and back. Keep blades down and back as you bring arms to a "T" with thumbs pointed up. Then bring arms to a wide "Y" with thumbs up. Back to the "T" and then back to side. Don't let low back arch. Actively press shoulder blades downward toward hips through the movement. Can also bring knees to floor if having difficulty maintaining posterior pelvic tilt. Self Myofascial Release Purpose: decrease pain and improve mobility of soft tissue to scapular and rotator cuff musculature to facilitate normal scapular mechanics. Posterior Rotator Cuff Instructions: Stand with tennis ball pressed between back side of shoulder blade and wall. Find tender or tight spot, pin it with the tennis ball and then passively or actively move the involved arm (upward or across chest) until muscles relax. Pectorals Instructions: Facing a doorframe, place tennis ball between pectoralis muscle and doorframe with arm in “cactus position” or at side. Slowly turn sternum away from ball until feel stretch in chest. Upper Trapezius/ Levator Scapula Instructions: In door frame, place ball between doorframe and upper trapezius. Pin the tight areas and gently move neck until you feel muscles relax. References [1] Stocker D, Pink M, Jobe FW. (1995). Comparison of shoulder injury in collegiate- and master’s-level swimmers. Clin J Sport Med 5 (1): 4-8.
[2] Sein ML, Walton J, Linklater J, Appleyard R, Kirkbride B, Kuah D, Murrell GAC. (2010). Shoulder Pain in elite swimmers: primarily due to swim-volume-induced supraspinatus tendinopathy. Br J Sports Med 44(2): 105-13. doi: 10.1136/bjsm.2008.047282 [3] Su KP, Johnson MP, Gracely EJ, Karduna AR. (2004). Scapular rotation in swimmers with and without impingement syndrome: practice effects. Med Sci Sports Exerc 36(7): 1117-23. Who knew that something that comes so naturally can be used to help so many things such as your heart, brain, digestive system, immune system, and even improve your posture! I just came across an old episode of Morning Edition on NPR from 2010, in which a Harvard researcher, Herbert Benson, had research showing that breathing could affect gene expression.
The article he was referring to is titled “Relaxation Response Induces Temporal Transcriptome Changes in Energy Metabolism, Insulin Secretion and Inflammatory Pathways”. Now, I would never claim to understand anything about genome research and transcriptional profiling, but I found it an interesting read. My only knowledge on this subject probably comes from watching Law and Order and from living through the O.J. trial. (if you are not old enough to have ever seen a pay phone, there once was this famous football player…..oh never mind, look it up; I think there was a documentary about it at SXSW). The article explains that the “relaxation response” (RR) is a state that is the exact opposite of our “fight-or-flight” response. This state can be achieved in a number of ways: focusing on breathing, a word, phrase, sound, repetitive prayer or movement and disregarding everyday thoughts. This technique is a part of many different mind-body approaches such as meditation, yoga, Tai Chi, Qi Gong, progressive relaxation, and biofeedback. In this study, the researchers worked with both experienced relaxation practitioners and novice practitioners before and after receiving 8 weeks of relaxation training. The researchers looked at changes in genomic expression during a single session of RR. The specifics of the data collection and statistical analysis are beyond my pay grade, so fast-forward to the discussion. The researchers found changes in gene expression with both the experienced and the trained novices after a single RR session. The genes involved are those responsible for processes in the body that affect how our body produces energy and how our cells age. What was the intervention that the researchers used to cause this effect? The longterm practitioners reported regular practice of some sort of RR-inducing technique including several forms of meditation, Yoga, or repetitive prayer; so they just kept doing what they usually do. The novices had a weekly session where they were guided through an RR-inducing sequence: diaphragmatic breathing, body scan, mantra repetition, and mindfulness meditation. They also received a 20-minute audio CD that guided them through this same sequence once a day at home. Diaphragmatic breathing: 1. Lie on your back on rug or blanket on the floor in “dead man’s pose” with your legs straight and slightly apart, arms at your side but not touching your body, palms up and eyes closed 2. Bring your attention to your breathing. Take note of the depth of your breath, if you are breathing more into the chest or your abdomen. 3. Place one hand on your chest and the other on your abdomen. Breathe through your nose. Spend a minute or two breathing into your abdomen and letting your chest follow the movement of your abdomen. Body scan: As you continue the diaphragmatic breathing, systematically scan your body for tension. Start at the top of your head and move down from there, relaxing your face, your jaw, your throat, and your neck. Then progress to shoulders, arms, hands, chest, stomach, back, hips, legs and feet. You can imagine that your body is like a wick and every inhale draws a warm liquid (or cold liquid if it is mid-August in Austin) in through the top of your head. Every exhale pulls the liquid further down your body, breath-by-breath relaxing each part of your body and imagining each part feeling saturated and heavy. Mantra repetition: Mantra is a syllable, word or name that is repeated many times as you free your mind of thoughts. You can choose any word that has meaning for you “peace”, “love”, “calm”, or whatever holds meaning for you. Once you are settled into a quiet state, you chant the mantra aloud (but not so loud that it strains your voice). Focus on your word as you rhythmically speak it in a relaxed manner. You can then shift from chanting aloud to whispering it, relaxing even deeper. Mindfulness meditation: Sitting or lying quietly with eyes closed. Listen to the sounds around you. Give equal attention to each of them, no one sound being more significant than the other. Do not analyze or focus on any one sound. 1. say to yourself, “I am aware of all the sounds that surround me” 2. start this practice in a quieter location, but progress to louder, more crowded locations 3. once you are practiced at being aware of the sounds around you without focusing your attention on any one sound, then progress to allowing your thoughts to surface and listen to them without forcing them, analyzing them, or judging them. Observe them objectively without being influenced by them. Say to yourself, “I am aware of my thoughts, my perceptions of my environment and my body and my feelings. In this moment and this place I am experiencing these things. I have my own life and I am experiencing it right now”. 4. You can experience these thoughts from a relaxed, alert, impartial position. Twenty minutes a day and within 8 weeks, we can all make a positive impact on our brains and our bodies! Are you dealing with pain or injury? Learning these techniques are also an important aspect of teaching your brain not to "catastrophize" your pain experience and worsen your pain. Check out this book, The Opioid-Free Pain Relief Kit: 10 Simple Steps to Ease Your Pain by Beth Darnall, PhD. Order here on Amazon. References: Bhasin MK, Dusek JA, Chang B-H, Joseph MG, Denninger JW, et al. (2013) Relaxation Response Induces Temporal Transcriptome Changes in Energy Metabolism, Insulin Secretion and Inflammatory Pathways. PLoS ONE 8(5): e62817. doi:10.1371/journal.pone.0062817 Davis M, McKay M, Eshelman E (1982) The Relaxation & Stress Reduction Workbook. Oakland, CA: New Harbinger Publications. In May 2016, the US Food and Drug Administration (FDA) issued a warning about the use of a particular type of broad-spectrum antibiotics: Fluoroquinolones. In this statement, the FDA recommends that patients not be treated with fluoroquinolones for uncomplicated infections such as sinusitis, bronchitis or urinary tract infections due to the risk of "disabling and potentially permanent adverse events." The risks associated with these antibiotics include tendonitis, tendon rupture, central nervous system effects, peripheral neuropathy, myasthenia gravis exacerbation, QT prolongation and torsades de pointes (abnormal heart rhythms that can lead to sudden cardiac death, phototoxicity, and hypersensitivity. Fluoroquinolones include:
In a review of the research literature (Lewis, 2014), the author finds that the achilles tendon was affected in 95% of the fluoroquinolone-induced tendinopathy or tendon tears, but is also seen in tendons of the knee, hip and shoulder. The risk seems to be increased if the fluoroquinolone is used along with a corticosteroid (a 46-fold increase in risk). It is also important to note that the symptoms of the fluoroquinolone-induced tendinopathy can be seen as soon as a few hours after starting the medication and as delayed as much as 6 months after discontinuing antibiotic treatment. As an athlete:
For the Sports Medicine provider, it is important to know that, according to a case study (Greene, 2002), a fluoroquinolone-induced tendon injury may not respond to eccentric treatment like other tendinopathies, and may require a period of rest prior to progression to eccentric protocol. ReferencesFDA Statement
https://www.fda.gov/downloads/Drugs/DrugSafety/UCM500591.pdf Lewis T. Fluoroquinolones and Tendinopathy: A Guide for Athletes and Sports Clinicians and a Systematic Review of the Literature. JAT 2014:49(3):422-427 Greene BL. Physical therapist management of fluoroquinolone- induced Achilles tendinopathy. Phys Ther. 2002;82(12):1224–1231. |
AuthorKendal Jacobson, PT Archives
January 2023
Categories |
|
P 512-736-6742
F 877-736-5233 10601 Pecan Park Blvd, Suite #302 Austin, Texas, 78750
|
|




 RSS Feed
RSS Feed